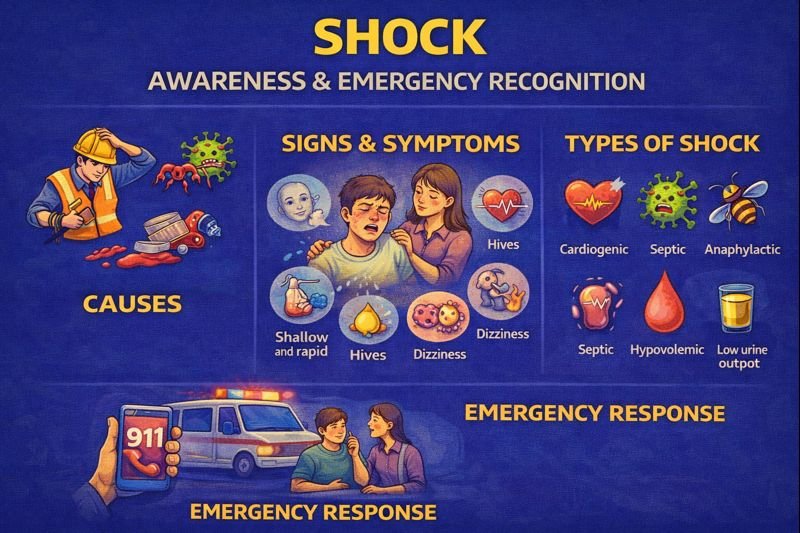
Shock: Causes, Signs & Emergency Recognition (Canada)
Why awareness matters in Canada
Shock can occur after trauma, allergic reactions, illness, blood loss, heat-related illness, or infections. It may arise in workplaces, sports environments, road collisions, outdoor settings, or at home. First aid and health awareness programs emphasize early recognition of shock rather than diagnosis.
Scenario
During a workplace construction project, a coworker fell and struck their leg. Shortly afterward, they became pale, dizzy, and unsteady. Their colleagues called emergency services, reassured them, and waited for paramedics to arrive.
Common signs & symptoms
Symptoms can vary depending on the underlying cause. Possible signs may include:
-
Pale, cool, or clammy skin
-
Fast breathing
-
Weak or rapid pulse
-
Dizziness or faintness
-
Nausea or vomiting
-
Anxiety or restlessness
-
Confusion or decreased alertness
-
Low blood pressure (determined by health professionals)
-
Chest discomfort
-
Reduced urine output (often identified in hospital settings)
-
Fever (in septic shock)
-
Hives, swelling, or breathing difficulty (in anaphylactic shock)
Not all signs appear at once, and some may be subtle in early stages.
Types of shock
Several medical conditions can lead to shock, including:
Hypovolemic shock
Related to significant fluid or blood loss.
Cardiogenic shock
Caused by the heart not pumping effectively.
Septic shock
Caused by severe infection affecting circulation and organs.
Anaphylactic shock
Caused by a severe allergic reaction involving breathing and circulation.
These conditions require diagnosis and treatment by trained healthcare professionals.
Possible causes
Shock may result from:
-
Trauma or bleeding
-
Severe dehydration
-
Infection
-
Heart-related problems
-
Medical complications
-
Extreme heat exposure
-
Certain diseases or medications
First aid awareness
Members of the public should focus on:
-
Calling emergency services when shock is suspected
-
Keeping the person calm and monitored
-
Observing for changes in breathing or alertness
-
Avoiding unnecessary movement if injuries are suspected
Healthcare professionals manage shock in clinical settings using oxygen therapy, fluids, medications, and other interventions depending on the cause.
Prevention & workplace considerations
Prevention strategies may include:
-
Protective equipment in sports and workplaces
-
Fall prevention and safe lifting practices
-
Heat safety measures for outdoor workers
-
Allergy plans for individuals at risk of anaphylactic reactions
-
Infection control and early medical care for illnesses
Canadian employers often include shock and trauma recognition in first aid training programs.
FAQ
Is shock the same as fainting?
No. Fainting is often brief and caused by reduced oxygen to the brain. Shock involves broader circulatory issues and requires medical attention.
Can anyone diagnose shock?
Diagnosis is made by healthcare professionals. The public focuses on recognizing concerning symptoms and calling for help.
Does shock always involve blood loss?
No. Infection, allergic reactions, and heart problems can also lead to shock.
Can shock develop slowly?
Sometimes. Septic shock and dehydration-related shock can develop over hours, while trauma-related shock may develop quickly.
Is shock treatable?
Yes. Treatment depends on the underlying cause and is provided in a hospital or advanced care setting.
Educational note
This material supports public first aid awareness. Individuals with concerning symptoms or suspected shock should receive prompt emergency medical evaluation.
