Shin Splints: Causes, Symptoms & First Aid Awareness (Canada)
First aid & workplace relevance
In Canada, shin splints show up in:
-
School and community sports (running, soccer, basketball, dance)
-
Military and police fitness training
-
Recreational running and walking groups
-
Workplaces involving repetitive walking, standing, or carrying loads
Understanding how shin splints develop, how to respond early, and how to reduce strain can help keep people active and safe at school, at work, and in sport.
Scenario
Jordan starts a new fitness routine and quickly increases running distance over two weeks. During a shift at their retail job, they notice a dull ache along the front of both shins that worsens when walking quickly or climbing stairs. They speak with a supervisor, adjust their duties for a few days, and schedule time with a healthcare provider to review footwear and training habits.
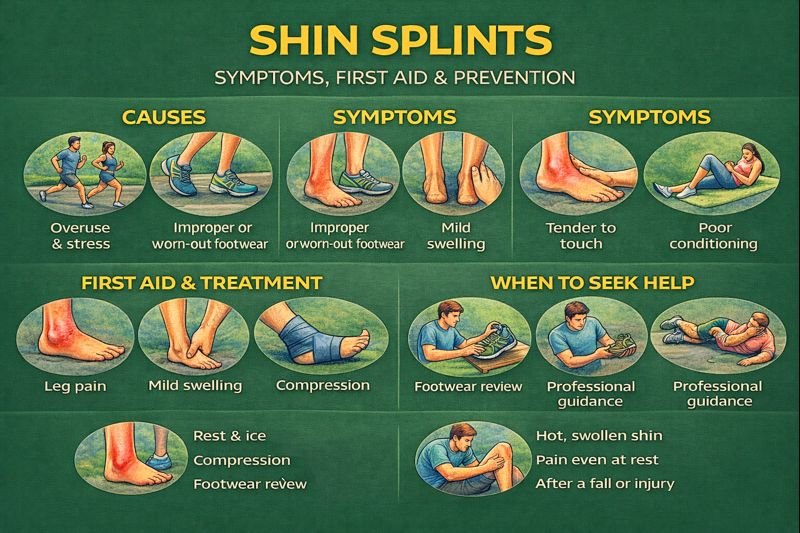
Symptoms of shin splints
People with shin splints may notice:
-
Dull, aching pain along the front or inner side of the lower leg
-
Pain that starts during exercise and can lessen with rest
-
Tenderness when pressing along the shinbone
-
Mild swelling in the lower leg
-
Tightness, fatigue, or weakness in the feet or ankles
Pain is usually felt in both legs, but can be one-sided. Symptoms often develop gradually as training or workload increases.
Causes & mechanisms
Shin splints are usually an overuse injury. Repeated stress on the shinbone and the tissues that attach muscles to bone can lead to irritation and inflammation.
Contributing factors can include:
-
Sudden increase in activity (time, speed, hills, or intensity)
-
Running or jumping on hard surfaces
-
Improper or worn-out footwear
-
Flat feet or high, rigid arches
-
Tight or weak muscles in the calves, hips, or thighs
-
Incorrect training technique (poor form, lack of warm-up)
-
Limited rest between training sessions
In some cases, repeated stress can create small bone “stress reactions.” Without adequate rest and recovery, these can progress to stress fractures.
First aid / management awareness
For suspected shin splints, public-level first aid focuses on reducing strain and supporting recovery:
-
Rest or modify activity
Reduce high-impact activities (running, jumping) and switch temporarily to lower-impact options such as walking, cycling, or swimming. -
Ice or cool packs
A cool pack wrapped in a cloth may be used on the painful area for short periods to help with discomfort. -
Elevation
Elevating the legs after activity can help with mild swelling. -
Footwear review
Consider whether shoes are worn out, unsupportive, or not suited to the activity. Health or footwear professionals can advise on appropriate options. -
Professional guidance
A healthcare or rehabilitation professional (e.g., physiotherapist) can assess biomechanics, muscle strength, and training habits, and suggest stretching, strengthening, or form adjustments.
Medication choices, if any, are best discussed with a health professional who knows the individual’s health history.
Prevention & workplace considerations
Prevention strategies can benefit athletes, students, and workers:
-
Gradual training progress
Increase distance, intensity, and frequency slowly rather than all at once. -
Warm-up and cool-down routines
Include light cardio and dynamic stretching before activity; gentle stretching afterward. -
Supportive footwear
Use activity-appropriate shoes and replace them regularly, especially for running and high-impact work. -
Surface awareness
Where possible, train on softer surfaces (tracks, trails) instead of only concrete or asphalt. -
Strength and flexibility
Strengthening hips, calves, and core, and maintaining flexibility in the lower body can help distribute load more evenly. -
Workplace ergonomics
For jobs with prolonged standing or walking, employers may consider anti-fatigue mats, rest breaks, and safe workload planning.
FAQ
1. Are shin splints the same as a stress fracture?
No. Shin splints involve irritation of bone and soft tissues, while stress fractures are small cracks in the bone. Only a health professional can distinguish them with proper assessment and, when needed, imaging.
2. Do shin splints always mean I have to stop all activity?
Not necessarily. Many people reduce high-impact activities and switch to lower-impact exercise while they recover, guided by a healthcare provider or therapist.
3. Can teenagers get shin splints?
Yes. Teens involved in sports, dance, or fast increases in training volume can experience shin splints, especially during growth spurts.
4. When should someone see a doctor for shin pain?
If pain is severe, persists despite rest, is present even at rest or at night, or follows a fall or impact, medical assessment is recommended to rule out stress fractures or other conditions.
5. Do shin splints go away on their own?
Many cases improve with rest, activity modification, and prevention strategies. Ongoing or recurrent pain should be evaluated by a health professional.
Educational note
This article is intended for general first aid and injury-prevention education. It does not replace assessment, diagnosis, or treatment from a qualified healthcare professional.
