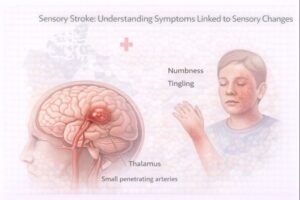
Sensory Stroke: Understanding Symptoms Linked to Sensory Changes
In Canada, stroke remains a major cause of disability and early medical care can dramatically reduce long-term complications. Public training in first aid and CPR, combined with AED access in workplaces and public spaces, continues to play an important role in early emergency response.
Lacunar Infarction & Sensory Symptoms
A lacunar infarction involves a blockage of a very small artery deep within the brain. These small vessels supply deeper brain structures such as the thalamus, which plays a major role in processing sensory information.
Damage in these regions can cause:
-
sudden numbness or tingling
-
altered temperature sensation
-
facial or eye movement changes
-
sensory disturbance on one side of the body
Although less common than larger ischemic strokes, lacunar strokes can still lead to long-term disability.
Hemorrhagic Stroke & Sensory Effects
A hemorrhagic stroke occurs when weakened blood vessels rupture and bleed into surrounding tissues. In rare cases, hemorrhage in specific brain regions (such as the thalamus or pons) can cause a pure sensory stroke with symptoms related mainly to sensation rather than muscle weakness.
MRI and other imaging are used to confirm the location and extent of bleeding.
Dejerine–Roussy Syndrome
Some survivors develop Dejerine–Roussy syndrome (thalamic pain syndrome) following a stroke involving the thalamus. This condition may lead to:
-
changes in pain perception
-
burning, freezing or discomfort with normal touch
-
temperature sensitivity
Not every individual develops this condition, but when present it may require long-term medical management.
Lifestyle & Risk Factors
Several risk factors can increase the likelihood of sensory complications after stroke, including:
-
high cholesterol
-
smoking
-
high blood pressure
-
excessive alcohol use
-
diets high in saturated fats
-
uncontrolled diabetes
A buildup of cholesterol plaque can narrow or block arteries, and weakened vessel walls can contribute to aneurysms and bleeding.
Learning Note
Early recognition of stroke symptoms and rapid activation of emergency medical services can improve outcomes. Community CPR and AED training, along with workplace safety programs, support faster response and better survival rates in sudden medical emergencies.
Educational Disclaimer
This article is for public education only and not for diagnosis or medical decision-making. Stroke and neurological symptoms require urgent professional assessment. If a stroke is suspected, call emergency services immediately.
