Whiplash Injuries: Causes, Symptoms & First Aid Awareness (Canada)
Why awareness matters
Whiplash injuries range from mild stiffness to more persistent discomfort. Symptoms do not always appear right away and may develop gradually over hours or days. Recognizing changes early helps ensure appropriate care and monitoring.
Scenario
After a low-speed bumper tap at an intersection, a commuter felt fine at first. Later that evening, they noticed neck stiffness and reduced range of motion. A family member suggested booking a medical assessment the next day to confirm no other related injuries.
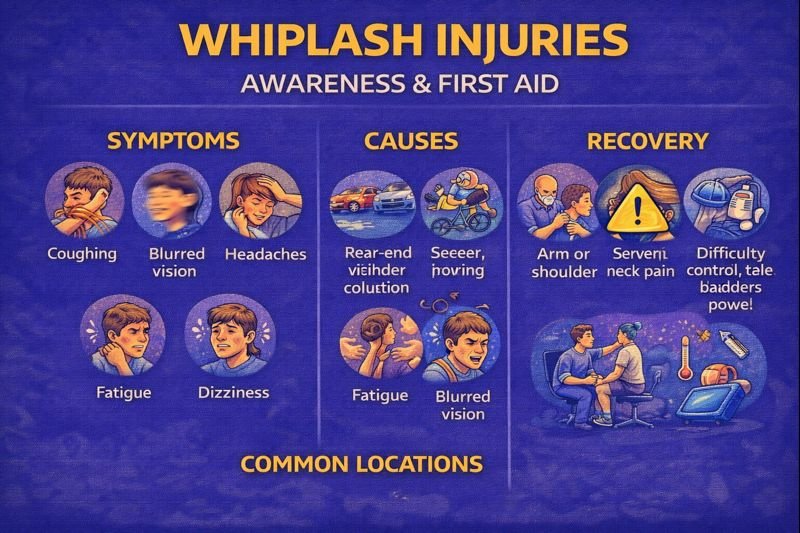
Common symptoms
Symptoms may appear within 24 hours but can sometimes take a few days to develop. They may include:
-
Neck stiffness or soreness
-
Reduced range of motion
-
Headaches (especially near the base of the skull)
-
Fatigue
-
Dizziness
-
Blurred vision
Less common symptoms that may appear with prolonged irritation include:
-
Ringing in the ears
-
Difficulty concentrating
-
Irritability or sleep disruption
-
Memory difficulty
When to seek medical assessment
A health professional should assess:
-
Symptoms involving the arms or shoulders (tingling, numbness, or weakness)
-
Pain that significantly limits neck movement
-
Symptoms that worsen rather than improve over time
-
Head injury concerns
-
Changes in coordination, bladder function, or bowel control
These features can help rule out more serious injury involving nerves or the spine.
Causes & risk scenarios
Whiplash can result from:
-
Vehicle collisions (especially rear-end)
-
Contact and impact sports (e.g., hockey, football, martial arts)
-
Cycling incidents or sudden stops
-
Horseback riding falls
-
Slips, trips, and falls
-
Playground or recreational injuries
Workplaces with warehouse equipment, vehicle fleets, or physical labour sometimes include whiplash awareness in safety programs.
Assessment & diagnosis
Health professionals may:
-
Take a detailed history of the event
-
Perform a physical examination of the neck and shoulders
-
Evaluate range of motion and strength
-
Request imaging (X-ray, CT, or MRI) when needed to rule out other injury
First aid & recovery awareness
Recovery strategies vary by individual and are guided by healthcare professionals. Approaches may include:
-
Early mobility and gradual return to normal activities as tolerated
-
Guidance from physiotherapists or rehabilitation professionals for flexibility and strength
-
Posture and ergonomics education to reduce strain during healing
-
Heat or cold applications for comfort, as recommended by a health professional
-
Medication decisions made by a doctor or pharmacist based on personal health history
Many mild cases improve over days to weeks, while some may benefit from ongoing therapy to restore movement and comfort.
Workplace & sport considerations
Organizations may address whiplash within:
-
Vehicle safety programs
-
Collision reporting procedures
-
Helmet and protective equipment policies
-
Return-to-play or return-to-work guidelines
-
Ergonomics and posture training
FAQ
Does whiplash always hurt right away?
No. Some people notice symptoms hours or even days later.
Can children or teens get whiplash?
Yes, especially through sports or collisions. Medical assessment helps guide safe recovery.
Is whiplash permanent?
Many people recover fully, but some may have lingering discomfort. Rehabilitation can help restore function.
Do all vehicle collisions cause whiplash?
Not always. Risk depends on speed, direction of impact, seating position, and headrest alignment.
Can posture affect whiplash recovery?
Good posture and ergonomics may reduce strain during healing and are sometimes included in rehabilitation plans.
Educational note
This article supports public first aid and injury awareness. Diagnosis, rehabilitation, and medication decisions are made by qualified healthcare professionals based on individual needs.
