Tibia Stress Fractures: Awareness, Symptoms & Activity Considerations
Relevance in Sports, Workplaces & Canadian Settings
Tibia stress fractures are commonly linked to athletics (running, dance, sport conditioning), military training, and occupations involving repetitive load or long periods of walking or standing. Awareness of stress fractures allows individuals, coaches, teachers, and supervisors to recognize signs early and encourage assessment before the injury progresses.
Scenario: Mild & Realistic
A high-school athlete started cross-country running after summer break. After a few weeks, they noticed throbbing discomfort along the shin after practice that gradually persisted during class and walking home. A healthcare provider later confirmed a tibia stress fracture and recommended activity modifications while the bone healed.
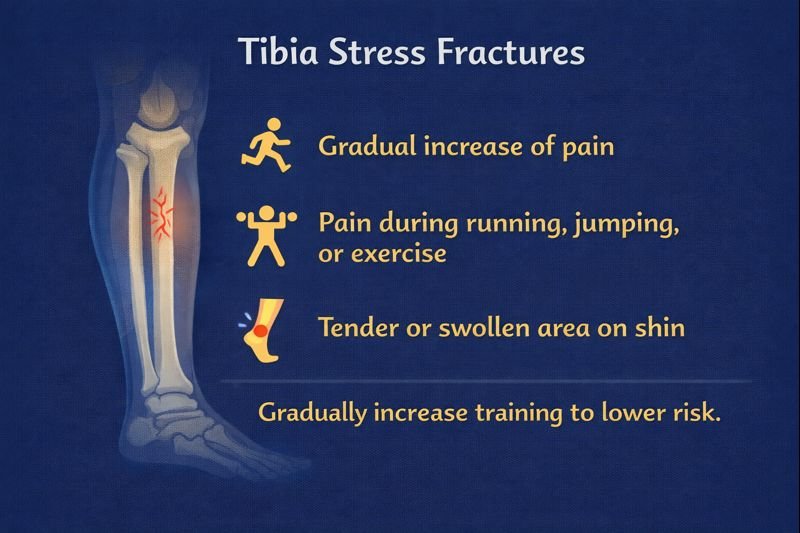
Possible Symptoms of Tibia Stress Fractures (Awareness Only)
Gradual Onset of Pain
Pain often begins mildly and increases over time. Early discomfort may be described as an irritation rather than sharp pain. Physical activity can worsen symptoms; walking or stairs may begin to feel uncomfortable as the condition progresses.
Activity-Linked Pain Patterns
Pain is frequently triggered by impact activities such as:
-
Running
-
Jumping
-
Weighted exercise
-
Long walks
-
Certain yoga or dance movements
In early stages, pain may ease with rest. As the stress fracture worsens, pain may persist during normal daily activities or even at rest.
Tenderness & Local Swelling
A specific spot on the tibia may become:
-
Tender to touch
-
Warm
-
Discoloured or bruised
-
Slightly swollen
Some individuals describe a localized “sore spot” or firmness along the bone.
Reduced Mobility or Performance
Flexibility and functional movement may be limited. Athletes might notice changes in gait, stride, strength, or balance. In severe cases, alignment and load patterns may change as the body avoids pain.
Risk Factors
Factors that may contribute include:
-
Sudden increases in training volume or intensity
-
Hard running surfaces
-
Poor footwear or limited shock absorption
-
High-impact sports (running, basketball, gymnastics, dance)
-
Overuse or insufficient rest
-
Bone density conditions (e.g., osteoporosis)
-
Nutritional factors and growth phases in younger athletes
-
Biomechanical imbalances (leg length differences, foot posture)
Children, teens, and young adults in growth periods can be especially susceptible during intense sport seasons.
Diagnosis & Care (Awareness)
Tibia stress fractures require medical assessment for diagnosis—often through imaging. Healthcare professionals guide:
-
Activity modification or temporary rest
-
Return-to-sport decisions
-
Strength and conditioning programs
-
Rehabilitation when appropriate
Early assessment may reduce healing time and prevent full fractures.
Prevention & Activity Considerations
Prevention strategies may include:
-
Gradual training increases
-
Appropriate footwear for sport & terrain
-
Strength and conditioning for legs & core
-
Alternating high-impact and low-impact activities
-
Ensuring rest and recovery time between workouts
-
Attention to biomechanics during adolescence growth spurts
Workplaces may reduce overuse injuries through scheduled breaks, footwear policies, and ergonomic considerations.
FAQ
1. Can you still walk with a tibia stress fracture?
Often yes, especially early on, which is why stress fractures can go unnoticed for weeks.
2. Is numbness common?
Numbness is less typical; pain is more common. Nerve-related symptoms should be assessed by a healthcare provider.
3. Do stress fractures heal quickly?
Healing time varies and depends on severity, age, and activity level. Healthcare providers guide return-to-activity.
4. Can teens and younger athletes get stress fractures?
Yes. Growth periods combined with training volume can increase risk.
5. Do stress fractures always show up on X-rays?
Not always. Healthcare professionals may use additional imaging if symptoms persist.
Educational Note
This information supports public education and injury awareness. It does not diagnose injuries or provide treatment instructions. Healthcare professionals determine appropriate care for suspected stress fractures.
