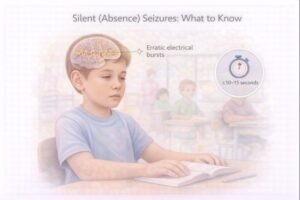
Silent (Absence) Seizures: What to Know
Understanding Silent (Absence) Seizures
Epilepsy describes a condition where unplanned bursts of electrical activity occur in the brain, leading to recurrent seizures. One form — often overlooked — is the silent or absence seizure. Unlike the more recognizable seizure types that involve muscular jerking, absence seizures may appear as brief moments of “tuning out.”
Silent seizures commonly affect children between 6–12 years old but can occur in teens and adults. Early recognition supports better school performance, safety, and long-term management.
Key Features of Absence Seizures
-
Sudden pause in movement or speech
-
Fixed staring or “blank” look
-
Mild lip smacking or small hand movements (in longer episodes)
-
Brief loss of awareness
-
No memory of the event afterward
Many episodes go unnoticed in busy environments such as classrooms, sports settings, or workplaces.
Why Do Silent Seizures Happen?
Absence seizures are driven by abnormal electrical signalling patterns in the brain. While the exact cause is not fully understood, researchers note a strong genetic component. They are also more common in childhood, potentially due to the developing nervous system having more active neural connections.
Diagnosis & Assessment
Healthcare providers may use the following tools to clarify the diagnosis:
-
Blood tests — rule out metabolic or electrolyte imbalances
-
Electroencephalogram (EEG) — detects the rhythmic activity pattern typical of absence seizures
-
MRI (when indicated) — rules out structural causes such as tumours
Timely assessment is valuable for learning and safety, since untreated absence seizures can affect academic and social functioning.
Treatment Options
Treatment for absence epilepsy often includes anti-epileptic medications (AEDs) that reduce seizure frequency or stop seizures completely. Commonly used medicines for absence seizures include:
-
Ethosuximide
-
Valproic acid
-
Lamotrigine
Medication plans are typically tailored to the individual. A healthcare provider will also discuss monitoring, routine follow-up, and safety precautions.
Learning, Safety & Daily Activities
Because absence seizures interfere with awareness, they can impact:
-
Driving eligibility (provincial regulations apply across Canada)
-
Workplace safety (especially safety-sensitive roles)
-
School learning and attention
-
Sports and physical activities
Most individuals with well-controlled absence seizures participate fully in education, recreation, sports and — in adulthood — occupational settings. Employers and educators may support success by recognizing brief staring episodes as neurological, not behavioural.
Workplace & Training Relevance (Canada)
Awareness of medical conditions, including seizure disorders, supports safer environments in Canadian workplaces. In first aid and CPR / AED training, seizures are a key topic because responders may encounter different seizure presentations.
While absence seizures are typically brief and do not require emergency care, training helps by:
-
Identifying when a seizure requires emergency medical attention
-
Supporting workplace incident recognition
-
Reducing stigma and misinterpretation
Educational Disclaimer (included as required)
This information is for educational purposes only and not a substitute for professional medical assessment, diagnosis, or care. Individuals with potential seizure symptoms should seek medical advice from a qualified healthcare provider.
