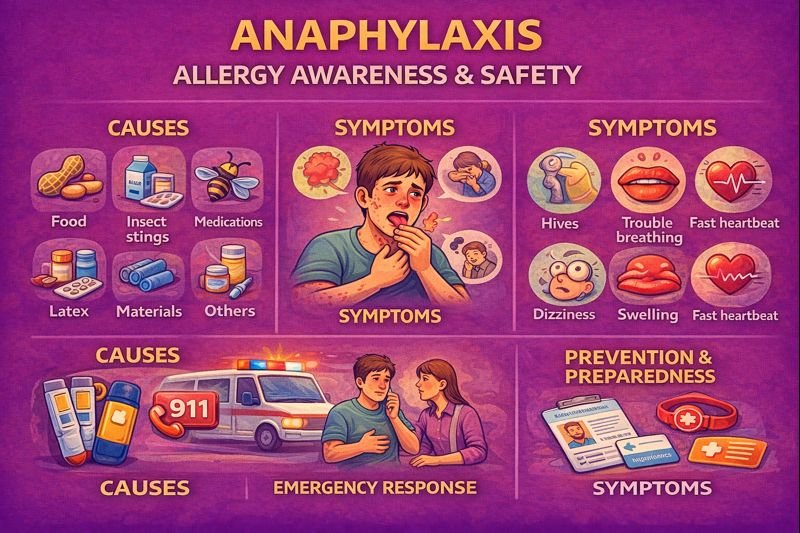
Anaphylaxis: Allergy Awareness, Signs & Emergency Recognition (Canada)
Why awareness matters
Food allergies, insect stings, and medication sensitivities affect Canadians of all ages. Schools, camps, daycares, workplaces, sports programs, and restaurants frequently manage allergy-related safety plans. Early recognition and prompt emergency response play an important role in anaphylaxis.
Scenario
During a family picnic, a teen experienced itching and hives shortly after eating. A caregiver checked their allergy plan, monitored the symptoms, and arranged medical care. Because the allergy was recognized early, the situation was handled calmly.
Causes & triggers
People with allergies may react to:
-
Certain foods (e.g., peanuts, tree nuts, eggs, milk, soy, shellfish)
-
Insect stings
-
Medications
-
Latex or other materials
Not all allergic reactions lead to anaphylaxis. Risk is higher for those with a known history of allergies or previous anaphylactic reactions.
Signs & symptoms of anaphylaxis
Symptoms may appear within minutes and can involve multiple body systems, including:
Skin & mucous membranes
-
Hives
-
Itching
-
Swelling (lips, tongue, face, hands)
Respiratory
-
Coughing
-
Difficulty swallowing
-
Tightness in the chest
-
Trouble breathing
-
Noisy breathing or wheezing
Gastrointestinal
-
Nausea or vomiting
-
Cramping
-
Diarrhoea
Cardiovascular & neurological
-
Dizziness or faintness
-
Weakness
-
Fast pulse
-
Low blood pressure
-
Confusion or reduced alertness
Patterns can vary. Some reactions have an early phase that resolves and later reappears—known as a biphasic reaction.
Emergency recognition
Call emergency services if anaphylaxis is suspected—especially if breathing, circulation, or consciousness is affected. Lay responders mainly focus on:
-
Staying with the person
-
Keeping them calm
-
Monitoring breathing and alertness
-
Activating emergency services promptly
Schools, workplaces, camps, and sports programs often include anaphylaxis response plans in their safety procedures.
Epinephrine auto-injectors & allergy plans
Many individuals at risk of anaphylaxis are prescribed epinephrine auto-injectors (e.g., for food allergies or insect stings). These devices are used according to a personalized plan created with a health professional. After use, medical assessment is still recommended.
Families, caregivers, coaches, teachers, and co-workers may learn how to recognize anaphylaxis and follow the individual’s allergy plan.
Prevention & daily management
Prevention strategies often include:
-
Identifying allergy triggers
-
Reading ingredient labels
-
Preventing cross-contact during food preparation
-
Communicating allergies in social and workplace settings
-
Carrying prescribed medications
-
Using medical identification bracelets or cards
Health professionals may use allergy testing to help identify specific triggers and guide avoidance strategies.
FAQ
Can anyone develop anaphylaxis?
Yes, although individuals with known allergies are at higher risk.
Do symptoms always look the same?
No. Symptoms vary and may affect skin, breathing, digestion, or circulation.
Is anaphylaxis rare?
It is less common than mild allergic reactions but taken seriously due to its potential severity.
Do workplaces and schools prepare for anaphylaxis?
Many Canadian schools, camps, and workplaces have allergy protocols and encourage training for recognition and emergency response.
Can anaphylaxis be prevented?
Trigger identification, communication, and avoidance strategies reduce risk for those with diagnosed allergies.
Educational note
This material supports public allergy and first aid awareness. Health professionals can provide personalized testing, prescriptions, and allergy plans based on individual needs.
