Animal Bites: First Aid Awareness, Infection Risks, and Workplace Safety in Canada
What Are Animal Bites?
An animal bite occurs when an animal’s teeth break or compress human skin or underlying tissue. Each year, millions of people worldwide experience animal bites, and many injuries involve the hands and fingers, particularly the dominant hand. Bites can also occur on the arms, legs, face, neck, or head, depending on the situation.
Animal bites range from minor surface wounds to deeper injuries that affect muscles, tendons, nerves, or bone. Even bites that do not break the skin can still cause significant internal damage.
First Aid and Workplace Relevance in Canada
Animal bites are relevant in many Canadian workplaces, including animal care, delivery services, public-facing roles, parks, healthcare, and home-based services. They can also occur during everyday activities such as walking outdoors or interacting with pets.
First aid training helps individuals respond safely to animal bites by controlling bleeding, reducing infection risk, and recognizing when medical evaluation is needed. Understanding public health considerations—such as rabies awareness—is also important in Canada.
A Simple, Realistic Scenario
While making a delivery, a worker is bitten on the finger by a startled dog at a private residence. The worker remembers their first aid training, cleans the wound once bleeding is controlled, covers it with a clean dressing, and reports the incident. They seek medical assessment later that day to ensure proper follow-up and documentation.
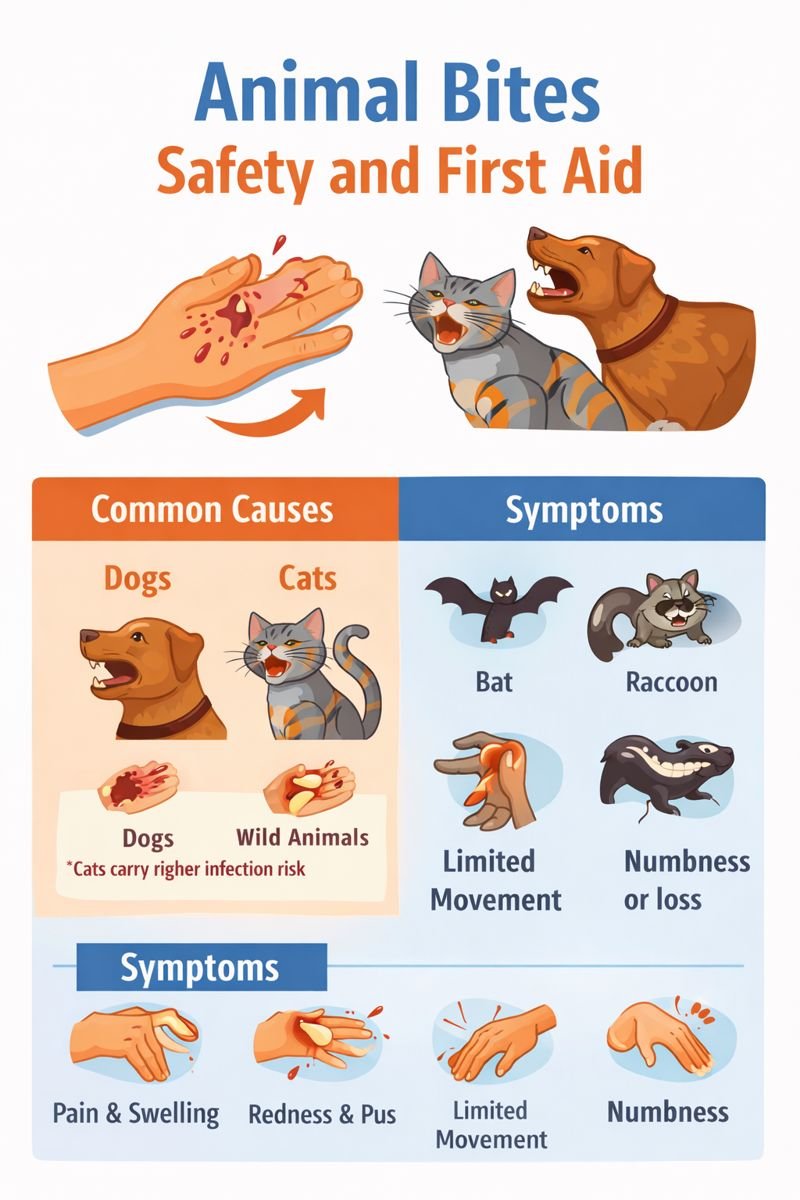
Common Causes of Animal Bites
Key concerns related to animal bites include:
-
Bacterial infection
-
Damage to tendons, nerves, or joints
In Canada and other developed countries, rabies is rare in vaccinated domestic pets. Most rabies cases are linked to wild animals, such as bats, skunks, raccoons, and foxes. In other parts of the world, dog bites remain a more common source of rabies.
Symptoms and Signs to Watch For
Animal bites may cause:
-
Pain, swelling, and bruising
-
Redness or warmth around the wound
-
Drainage or pus from the bite area
-
Limited movement or weakness near the injury
-
Numbness or loss of sensation
Even if the skin is not visibly broken, crushing or tearing injuries beneath the surface can affect muscles, tendons, ligaments, nerves, or bone. Difficulty bending or straightening a finger, or loss of feeling, may suggest deeper injury.
First Aid and General Management
From a first aid perspective, priorities include bleeding control, wound protection, and infection awareness.
General first aid considerations may include:
-
Using clean materials to control bleeding with gentle pressure
-
Avoiding contact between the wound and the mouth
-
Protecting the area with a clean, non-stick dressing
-
Monitoring for signs of infection or reduced function
Bite wounds should be observed closely during healing. Many minor wounds improve within 7 to 10 days, but delayed healing or worsening symptoms require medical evaluation.
When Medical Assessment Is Important
Medical care is often required if:
-
The bite breaks the skin
-
The wound is deep, painful, or heavily contaminated
-
There are signs of infection
-
Movement or sensation is affected
-
The bite involves the face, head, or neck
-
The bite is from a wild animal or an unknown animal
Healthcare providers may assess the wound, clean it thoroughly, and check for deeper damage. In some cases, imaging or blood tests may be used as part of evaluation. Animal bites involving wild species are typically reported to public health authorities for follow-up and rabies monitoring.
Prevention and Workplace Safety Considerations
Preventing animal bites involves awareness and risk reduction.
Helpful strategies include:
-
Avoiding contact with unfamiliar or agitated animals
-
Following workplace procedures when entering homes or outdoor spaces
-
Using protective equipment where appropriate
-
Reporting animal-related incidents promptly
-
Maintaining up-to-date first aid training
Education helps workers respond calmly and safely if a bite occurs.
Frequently Asked Questions
Are all animal bites likely to become infected?
Not all bites become infected, but broken skin and deeper puncture wounds carry a higher risk.
Why are cat bites more likely to cause infection than dog bites?
Cat bites often create deep puncture wounds that can trap bacteria under the skin.
Can an animal bite cause serious injury without breaking the skin?
Yes. Crushing or tearing injuries can damage underlying tissues even if the skin remains intact.
Is rabies a common concern in Canada?
Rabies is rare in domestic pets but can occur from contact with certain wild animals.
How does first aid training help with animal bite incidents?
First aid training teaches bleeding control, infection awareness, safe response, and when medical follow-up is needed.
Educational Note
This article is intended for general education and workplace first aid awareness in Canada. It does not replace medical assessment, diagnosis, or treatment following an animal bite.
